By Rebecca Adams
Roll Call
Many people get nervous any time they need to go to the doctor. But in the past year, some U.S. residents became more concerned than usual.
Immigrants around the country who are on edge about broader enforcement under the Trump administration have been skipping appointments, questioning whether enrolling in government-funded health care coverage could undermine their immigration applications and showing anxiety about visiting unfamiliar physicians, according to nearly two dozen medical providers and lawyers interviewed recently.
Isaura, an undocumented mother of two children living in the Washington, D.C., metro area, described the deep apprehensions some immigrants feel about venturing out in the current political climate.
“Now I feel scared to even go to a new doctor because you don’t know what can happen. You have to give all the information — give your address and personal information — and if I don’t know somebody, I don’t go,” Isaura said. Her older son is asthmatic and has allergies.
“I’m very nervous to go to a new doctor or new place because I’m scared to drive, and everyone else feels the same. Everyone feels threatened because the police can stop you,” said Isaura, who asked that her last name not be used.
So far, her family hasn’t had to visit a new physician. She feels comfortable taking her children to familiar clinicians that serve a large number of immigrants, but would be concerned about getting care elsewhere.
With fears of arrest causing undocumented residents to recalibrate their everyday lives — including fewer trips for medical care — the consequences could cascade beyond the immigrant population. Skipped vaccinations or treatments could hasten the spread of infectious diseases.
Avoiding treatment for chronic ailments invites a torrent of potential trouble, including more expensive and invasive care later. And when the patient is uninsured, those costs often are absorbed either by government health programs or by hospitals, which may cover the expense by hiking prices for insured patients.
“Immigrants are no more dangerous than anyone else, but when we craft policies that drive any population underground, it puts all of the rest of our health at risk, particularly for contagious diseases,” said Georges Benjamin, the executive director of the American Public Health Association.
Karen Mountain, the chief executive officer for the Migrant Clinicians Network, a nonprofit medical network, said thousands of clinicians are reporting higher no-show rates and a reluctance by immigrants, both those here legally and illegally, to get needed care.
“I’m in the business of trying to help people when they are ill, and I am unable to do that effectively when people are too afraid to seek care,” Mountain said. When patients are “scared to death” to seek even routine care, she adds, that “should be a concern to all taxpayers.”
Among those affected are children, including many born in America: 88 percent of children living with an immigrant parent are U.S. citizens.
Sensitive issues
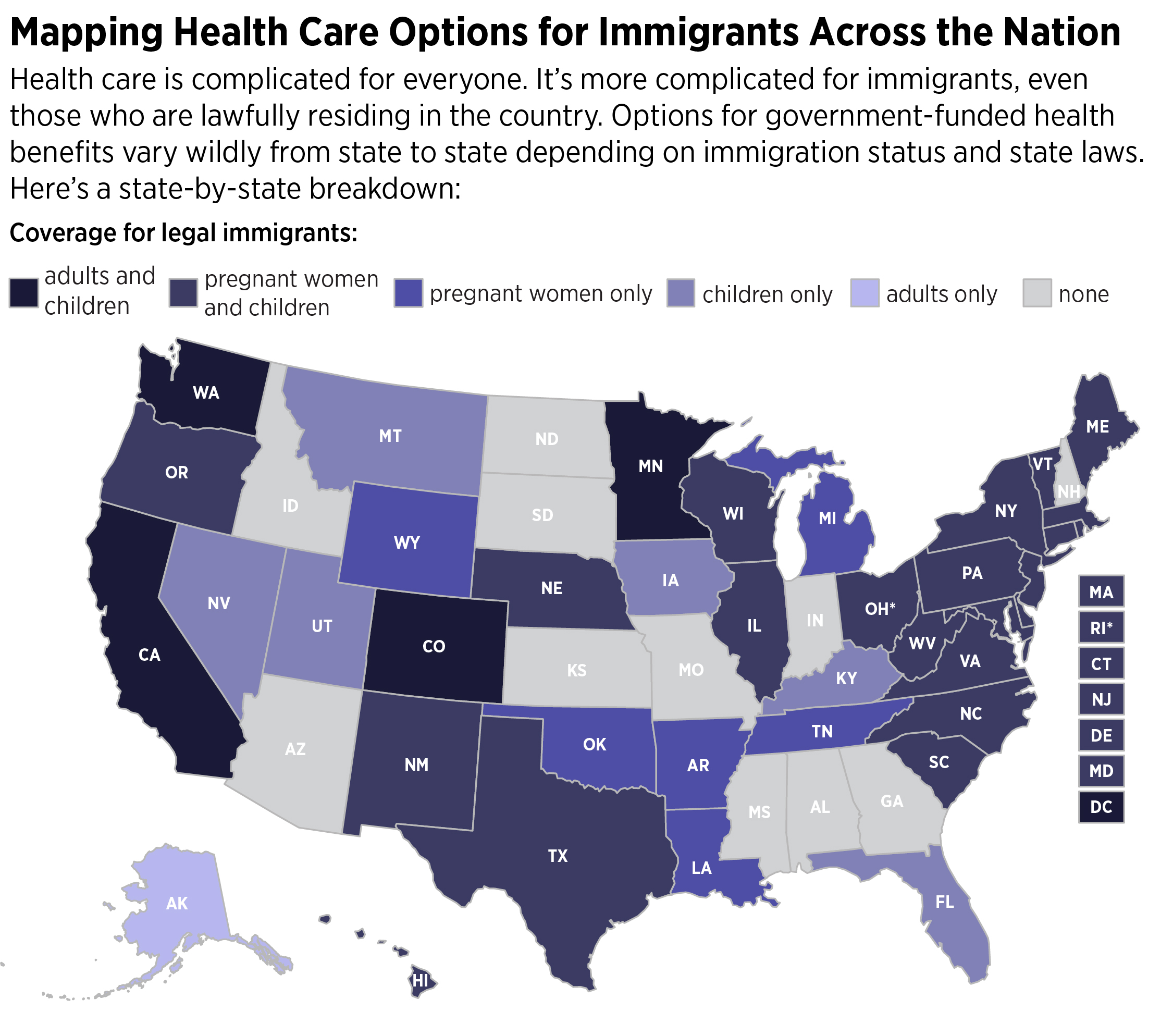
The concerns are emerging against a backdrop of abruptly changing policies for the approximately 23 million legal and undocumented immigrants that account for about 7 percent of the U.S. population.
The Trump administration in its first year ended protections for about 330,000 people who were legally allowed to live in the United States under temporary protected status because of natural disasters, wars or other problems in their home countries. Many have lived here for decades.
President Donald Trump also overturned protections for about 690,000 young people, often called Dreamers, who came to the country as children and were allowed to work in the U.S. through the Deferred Action for Childhood Arrivals program. Democrats and Republicans are now debating whether to enshrine the DACA protections into law, roll back Trump’s decisions for several groups and boost border security as part of a deal.
Trump’s policies followed a stronger enforcement effort and more deportations under President Barack Obama. But Obama prioritized felons, those tied to gangs or terrorists, and people crossing the border, while Trump’s priorities are far broader. He is giving immigration officials discretion to pursue any violators they find.
Hospitals or medical treatment facilities, schools, churches, and public demonstrations have been considered safe havens — “sensitive locations,” in the parlance of a 2011 U.S. Immigration and Customs Enforcement memo under the Obama administration. But over the past year, reports surfaced of agents targeting immigrants near these locations. The Trump administration says on the ICE website that agents may capture someone at a sensitive location “if there are exigent circumstances, if other law enforcement actions have led officers to a sensitive location, or with prior approval” from a supervisor.
In May, the parents of a 2-month-old with a condition that causes vomiting and weight loss were planning to take the baby, a U.S. citizen, to a Corpus Christi hospital a couple of hours from their Texas home. A Border Patrol officer who was tipped off showed up at the hospital where they were and offered them an escort past a checkpoint on the way, which was perilous because they were undocumented. The catch: they would be arrested and face deportation hearings. The four children of the couple, Oscar and Irma Sanchez, are American citizens.
In October, the case of a 10-year-old with cerebral palsy made headlines after she was stopped at a checkpoint on her way to the same hospital for emergency gallbladder surgery.
After the hospital released Rosa Maria Hernandez, who has lived in the U.S. with her undocumented parents since she was 3 months old, immigration officials sent her to a detention center that typically holds people caught crossing the border unlawfully. She was eventually returned to her family but faces deportation hearings.
Last year, Sara Beltran Hernandez, then 26, was awaiting surgery for a brain tumor when immigration officials found her at a Fort Worth, Texas, hospital. She had previously been detained because she was undocumented, and they returned her to custody.
Some medical facilities faced attempts to breach their “safe haven” even before the Trump administration.
In a previously unreported case, two undercover immigration officers tried in 2016 to pick up an immigrant at a clinic in the Washington, D.C., area. Each came in, initially pretending to be acquainted with the patient and asking if he was there, the clinic staff said. The staff made clear the information was private and the agents never made it past the front desk. Eventually, when one of the officials disclosed that he was an immigration agent, the staff turned him away and the officers left.
Worried that news of the incident would rattle other people needing medical care, the clinic kept quiet about it.

ICE spokeswoman Justine Whelan said the department would need the immigrant’s name, date of birth and other details in order to track down the incident and comment on it.
Federal health privacy laws help clinics and hospitals protect patients’ identities, but even in immigrant-friendly New York City, officials at the nation’s largest public hospital system could sense the fear and feel the impact.
“We have seen a decrease in visits to our hospital,” said Israel Rocha, CEO of NYC Health + Hospitals/Elmhurst. “Families are afraid to receive information and people leave their loved ones in the emergency room and run away.”
So the hospital network took steps to tamp down their patients’ fears and tell them it’s safe to come to the hospital. They put up reassuring signs in multiple languages and launched a broad publicity campaign. A series of hospital-sponsored community events encouraged immigrants to get insured and seek care when they need it.
A wide range of medical providers and attorneys in California, Georgia, North Carolina, New York, Texas and the D.C. metro area in separate interviews said that many of their clients who aren’t citizens, including some legal residents, are skittish about the changing conditions for immigrants and must be reassured that it is safe to get care or enroll in government-funded coverage they are eligible to receive. That’s particularly true if a patient has to leave a trusted community clinic to get follow-up treatment or tests at an unfamiliar hospital or doctor’s office.
Congressional Democrats introduced legislation to put the 2011 protections into law and expand the protected places to locations such as courthouses and motor vehicle offices. The legislation is unlikely to become law, but it raised the issue’s profile.
In an early January internal memo, Border Patrol Acting Chief Carla Provost said agents can expedite transit around a checkpoint during immediate emergency operations, and she reminded agents they can use their judgment about whether to take patients into custody. Officers should consider the sensitive locations policy before doing any follow-up interviews at a hospital, said Provost.
But she did not prohibit officials from taking patients at a medical treatment facility into custody. Border Patrol spokesman Carlos Diaz said in an email that the memo changed no policies and that people in ambulances will still be reviewed at checkpoints.
Jessica Vaughan, director of policy studies for the Center for Immigration Studies, which wants to limit immigration into the United States, said agents did the right thing in cases such as that of 10-year-old Hernandez.
They first need to make sure that the minor is cared for appropriately, she said.
“When the emergency is over, then the enforcement chips fall where they may,” Vaughan said. “The agents cannot ignore law-breaking happening right under their nose.”
Some legal residents worry about the administration’s shifting immigration policies. Besides the changes to people here under statuses that previously were protected, a draft executive order said to be under consideration last year by the Trump administration also provoked fear, although it was never finalized. Immigration advocates feared the order would have potentially made it harder for immigrants to get green card work permits if they enrolled in Medicaid.
For decades, immigration policy has held that immigrants seeking to enter the country or get a green card allowing them to work must show that they are unlikely in the future to rely on the government to survive. Officials evaluate applicants’ personal situations such as their age, health, income, assets, resources, education and skills, and family members who will support them or whom they will support. Currently, officials do not count it against applicants if the immigrants receive Medicaid, the federally and state-funded program for the poor and people with disabilities. But the executive order would have broadened the language, leaving advocates for immigrants concerned that officials could interpret it in a way that potentially would make it harder for people to get or keep green cards if they used federal benefits. Some advocates were concerned that people who sponsored immigrants might have to repay any benefits that were used.
“That’s when we started hearing these stories from patients saying they didn’t want to enroll their children, or they wanted to disenroll,” said Bill Phelps, chief of program services at Clinica Sierra Vista, a health care organization serving about 200,000 people in Fresno, Kern and Inyo counties in California.
The number of people failing to show up for scheduled visits also rose. The system’s “no show” appointments increased from 254,896 in 2016 to 270,383 in 2017, a 6.1 percent increase.
The number of people signing up for Women, Infants, and Children food assistance for low-income pregnant women, mothers of babies and children up to age 5 also dropped in the group’s centers, Phelps said.
The clinics’ WIC caseload dropped by an average of 2.6 percent from 2016 to 2017, continuing a trend in recent years. Phelps said he believes immigration issues played a part in the decreasing caseload, though it’s unclear how much.
Nationally, the WIC caseload has been declining in recent years and advocates say it continues to fall, although updated national data isn’t yet available.
Some say they have heard that immigration-related fears are part of that trend. Brian Dittmeier, the state government affairs counsel for the National WIC Association in Washington, D.C., said the organization received anecdotal reports of recipients asking if local WIC officials could not only stop their benefits but also remove their personal information from databases.
In a survey by the association of local and state WIC offices last year, 80 of 92 branches that responded reported signs of immigrants’ concerns, including a rising number of canceled appointments and questions about whether WIC participation would hamper the ability to get a green card or visa.
Benjamin, of the American Public Health Association, said that legal residents also may be discouraged from seeking care at some places if they feel they may be profiled and face hassles because of the current climate.
Some groups that want to curtail immigration, especially illegal immigration, say that outreach can ease concerns.
Vaughan, of the Center for Immigration Studies, said there is no reason that people in the country legally should fear seeking medical care and she hopes health care and advocacy groups are making that clear.
“People who are in the country illegally understandably may be reluctant to access health care services, especially if they cannot pay for those services,” she said.

Coverage drop for undocumented
National statistics that might reflect a decline in immigrants seeking medical care are scarce at this stage. Updated U.S. Census Bureau data on coverage for immigrants is not yet available. The federal Health Resources and Services Administration collects information about visits by all patients in community health clinics, which often serve legal and illegal immigrants, but 2017 data won’t be available until the fall. Neither HRSA nor trade organizations for providers such as the American Hospital Association publish statistics on canceled or no-show appointments. Hospitals and other providers say they do not track patients’ immigration status.
The Migrant Clinicians Network did survey its members last year. About 63 percent of the professionals who responded perceived a change in patients’ attitudes toward getting health care. Their explanations included responses such as “patients/clients seem to be more fearful of ICE and we’ve had to provide more reassurance regarding visiting the clinic” and “there is growing fear within the immigrant community due to the recent political climate.”
Legal residents can get government-subsidized health coverage under some conditions, such as waiting five years before qualifying for Medicaid. Federal Medicaid officials do not publish statistics on how many legal residents received coverage.
But statistics from some states that offer coverage to undocumented people do show a sharper-than-usual drop in that enrollment recently. California statistics reveal that Medicaid enrollment for undocumented adults has been falling more than the rest of the Medicaid population. From September 2015 until July 2017, the undocumented enrollment fell by about 4.4 percent statewide. The rest of the Medicaid population went in the opposite direction, growing by 2.7 percent, according to a Roll Call analysis of data from the state Medicaid program Medi-Cal. The biggest declines came after the latter half of 2016.
The drop was particularly striking in conservative parts of the state such as the Central Valley. In Fresno County, the undocumented group fell by 9,585 people, or almost 33 percent, from September 2015 to July 2017, while the rest of the Medicaid population in that county grew by 6 percent.
Its smaller neighbor, Kings County, saw a 37 percent decline, while the rest of the county’s Medi-Cal population rose by 5.3 percent over that timeframe. Other small counties saw drops of up to 41 percent in the undocumented Medicaid population.
The biggest increase in numbers of people came in an area that welcomes immigrants, Los Angeles County, where the undocumented population ticked up slightly by 1,917 people from September 2015 to July 2017. That was essentially flat at 0.5 percent growth. The overall Medicaid population there grew by 2.7 percent in that period.
The drop in coverage for undocumented people has not been previously reported.
“That might be indicative of the interaction of local policies, whether it’s police cooperation with ICE, county welfare offices being less welcoming, or the whole raft of things that might be happening as a result of county policies interacting with broader national trends,” said Steven Wallace, an immigration expert and associate center director at the Center for Health Policy Research at the University of California, Los Angeles.
Wallace said there wasn’t a huge exodus of immigrants in the Central Valley counties such as Fresno, or economic changes that would significantly boost immigrants’ income so that they would no longer qualify for Medicaid. It stands to reason that some immigrants are choosing not to enroll.
“Central Valley counties seem to be where you’re seeing a chilling effect, which would be consistent with the political resonance of the Central Valley,” Wallace said.
Other states don’t have county-level data but also show overall drops in coverage for undocumented people. Illinois showed a deeper drop in the undocumented population than the rest of the Medicaid population in every year of state data available for 2014 through 2017. For instance, the number of undocumented beneficiaries fell by nearly 8.3 percent from fiscal 2015 to fiscal 2017, while the population of other groups fell by 2.6 percent over that time period.
Illinois Department of Healthcare and Family Services spokesman John Hoffman said there were no health policy changes in recent years to explain the difference.
When parents are uninsured, they also are less likely to sign up their children for government-funded benefits, health policy experts say. A December 2017 Kaiser Family Foundation brief cited two studies showing that a parent’s coverage in public programs is associated with higher enrollment of children.
Hispanics, whether or not they are immigrants, start out as the ethnic group least likely to get coverage in America, with 16 percent of Latinos uninsured in 2016, according to census data. About 6 percent of whites and more than 10 percent of blacks were uninsured.
The nonpartisan Kaiser Family Foundation reported a decreasing use of some medical care and falling participation in federally and state-funded programs such as Medicaid and the Children’s Health Insurance Program due to immigration fears, according to findings published in December from focus groups of 100 parents born in 15 different countries. But the discussions in the focus groups, which were held in eight cities, also indicated that many parents kept their children enrolled in coverage and said “they highly prioritize their children’s health and generally view hospitals and doctors’ offices as safe spaces.”
Some parents said they are only leaving the house when necessary, such as for work, and are limiting driving, though, the Kaiser report found. “They and their children are spending long hours in the house behind locked doors,” the report said. Families “are increasingly fearful of interacting with police.”
Some clinicians say they suspect assaults or domestic abuse are increasingly not being reported to law enforcement. An October article in the Journal of the American Medical Association cited Los Angeles Police Department report statistics showing a 25 percent decline in the reporting of sexual assault between 2016 and 2017 among the city’s Latino population.

Weighing death vs. deportation
The health consequences for individuals and the broader population could be significant if residents grow more reluctant to receive care.
In New York, a woman with cancer who entered the country without documentation 20 years ago from the former USSR republic Georgia missed several appointments and told her doctor early last year she would not continue chemotherapy, according to Domna Antoniadis, an attorney for the New York Legal Assistance Group who assists patients in a New York hospital. She told Antoniadis that she felt Trump would deport her because she was receiving too much medical care. Antoniadis shared the story with the woman’s permission but declined to provide the patient’s name.
The woman, who has multiple myeloma, said she couldn’t return to Georgia without family ties there. Her family — including a sister who is a citizen, two children who qualified for DACA and a younger American-born son — live in the U.S. She worried her family might get in trouble if she pursued a relative petition for legal status.
She seemed to be weighing the risks of death versus deportation.
Her doctors feared that if she took her chemotherapy sporadically, it would not be as effective, her risks of drug resistance would rise and her likelihood of needing a stem cell transplant would increase.
She ended up stopping her treatment for four months despite encouragement to continue. When she returned after experiencing worsened symptoms and pain, she was tearful and depressed. She attended half of her scheduled appointments in recent months.
Antoniadis also shared three individual stories of patients with leukemia or lymphoma who had overstayed visas and were afraid last year to seek family petitions to get legal status. Each would have been eligible for treatment under state benefits while the applications were pending and if approved as expected. But because of concerns about the leaked executive order, two of the families were too afraid to apply, although Antoniadis repeatedly assured them the benefits would not count toward those considerations. The third patient’s son finally filed a family petition for his father after spending months consulting others.
All three patients died without getting treatment, Antoniadis said, because of incorrect perceptions about the executive order and whether family members would face repercussions if they applied for their relatives.
Effects on children
Not all of the issues clinicians are seeing are as harmful as missed cancer treatments, but still could impact people throughout life.
Julie Linton, a North Carolina pediatrician who co-chairs a special task force on immigration for the American Academy of Pediatrics, recently treated a newborn whose mother received little prenatal care after the father, who drove the woman to appointments, was deported. Another mother did not bring her baby in for several checkups because she was afraid to leave her home.
The stress of living with constant fear is also a threat to children’s health.
Scientists using technological advances from the past two decades can now peer into children’s brains with special MRI machines and literally map the results of chronic stress.
Researchers already knew that childhood stress leads to more health problems in adulthood. A major study by the Centers for Disease Control and Prevention and Kaiser Permanente through 1997 with more than 17,000 participants showed that as the number of adverse childhood experiences increased, including abuse or neglect or the separation of parents, the more likely children would grow up to face illnesses such as chronic obstructive pulmonary disease, alcoholism and heart disease.
In recent years, scientists have used brain scan images to show that the brains of people exposed to childhood stress sometimes look and appear to function differently than others. Studies have shown that these people often have smaller-than-normal volume in a part of the brain central to learning and memory; in another used in communication, emotional processes, and higher cognitive abilities; and in yet another that coordinates motor behavior and executive functioning. They often have a smaller prefrontal cortex, which is critical to behavior, cognition and the regulation of emotions. It may be harder for children and teens exposed to toxic stress to concentrate or to calm down after an alarming incident.
Doctors and nurses say children of immigrants show signs of stress, including headaches, trouble sleeping and dips in academic performance. The Kaiser foundation focus groups found that parents and pediatricians reported behavioral issues, such as problems eating; psychosomatic symptoms; and mental health problems among children. The report said pediatricians believed anxieties about immigration “served as triggers for parents who have histories of trauma or persecution” and some might face difficulties focusing on caregiving.
“We know that exposure to serious, prolonged stress, known as toxic stress, can harm the developing brain and threaten short- and long-term health,” Linton said. “We know that children who are exposed to serious early stress are more susceptible to heart disease, diabetes and depression.”
That could not only harm these families but also add to taxpayer-funded health care costs in the long run.
For undocumented parents like Isaura, questions about whether they might be deported and potentially be separated from their children are causing anxiety.
These concerns are consuming her thoughts, she said. “Everyone is very worried.”

Originally published in Roll Call on January 25, 2018.